|
Summary
Recent description of a
clinical syndrome of post-infarction “papillary muscle dysfunction”,
which is occasionally associated with severe mitral regurgitation,
prompted this experimental study. Extensive research was devoted to
studies of the spread of electrical activation in the myocardium in
animal experiments, but its spread in the papillary muscles in normal
and abnormal conditions was not studied in detail. We undertook a
study of activation in the anterolateral papillary muscle of
anesthetized, open-chest dogs. Recordings were obtained simultaneously
from four intramural multi-electrode needles inserted into the
myocardium at the base of the papillary muscle and directed towards
its apex. Baseline studies of the normal spread of activation
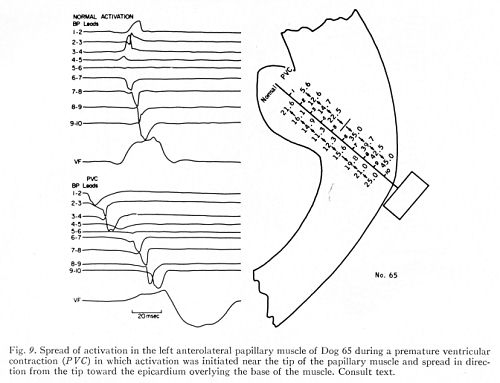
were performed in 30 dogs. Normal recordings were compared with those
obtained in spontaneously occurring premature ventricular
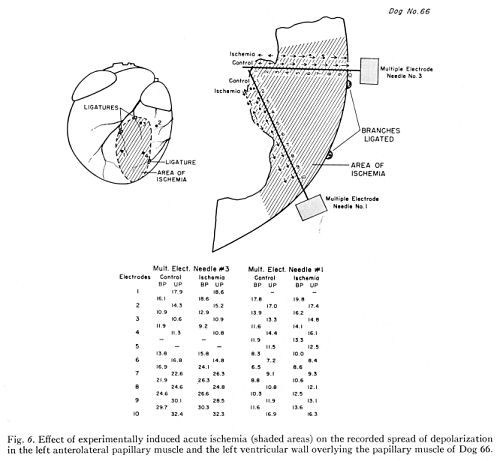
contractions. In 23 dogs, they were followed by induction of
localized ischemia by ligation of the small epicardial coronary
branches supplying the base of the papillary muscle. Progress of
ischemia was followed in 10 acute experiments for 4 to 5 hours.
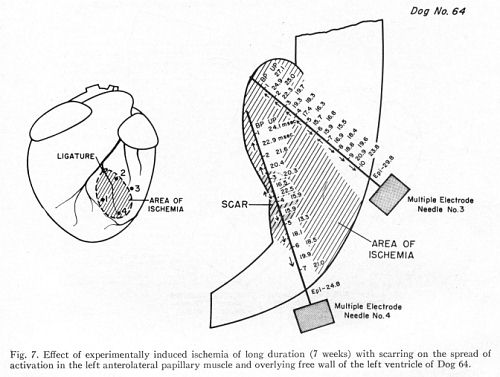
Ischemia of long duration with resulting scarring was
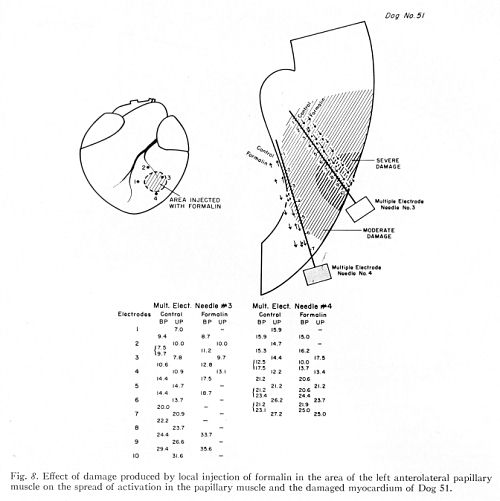
produced in 6 dogs and its results studied after 4 to 7 weeks. In 7
experiments, severe local damage was induced by intramyocardial
injecting of formaline solution mixed with staining dye for later
study of its extent and correlation with local electrocardiographic
changes. Serial electrocardiograms and vectorcardiograms were recorded
in all animals. Serial phonocardiograms were obtained in dogs with
induced localized myocardial ischemia.
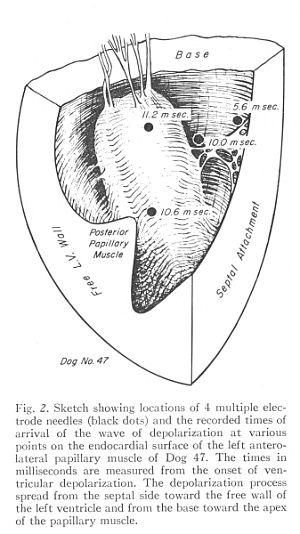
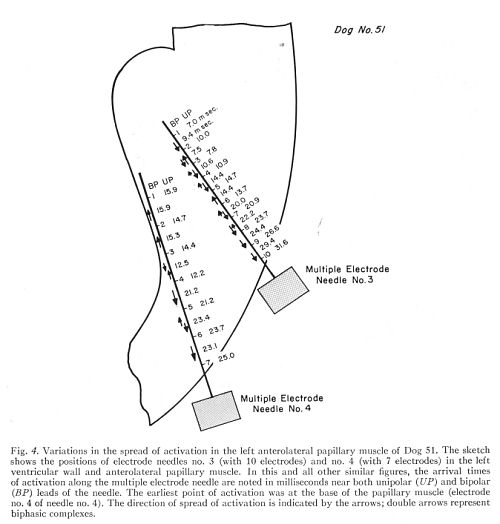
The endocardial wave of
activation was found to approach the papillary muscle from its septal
side and spread in the direction toward the free left vetricular wall
and toward the apex of the papillary muscle. The anterolateral
papillary muscle of the left ventricle was activated simultaneously by
the penetration of wave fronts: (1) from the endocardium into deeper
portions of the papillary muscle; and (2) from the central portions of
the papillary muscle and from the area of its attachment to the left
ventricular wall.
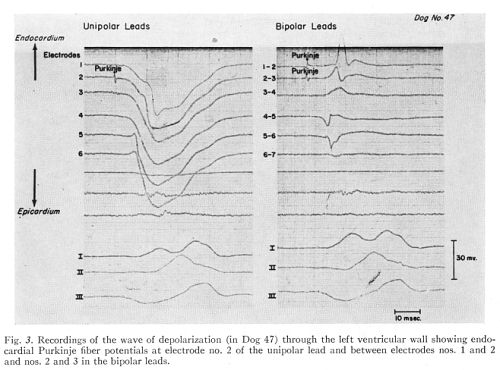
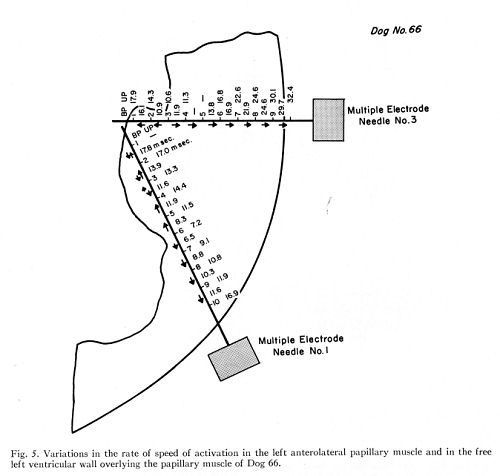
The shorter time needed for
the excitation wave to arrive at the epicardium in areas overlying the
papillary muscle and the higher calculated velocity of spread in these
areas indicate more abundant penetration of Punkinje tissue than in
the adjacent portions of the free left ventricular wall.
The pathologic influence on
the spread of activation in the papillary muscle was limited to the
time interval between 6 and 36 msec. of the cardiac electric cycle,
with no significant delays in the time of arrival of the process of
activation at the points of earliest activation within the papillary
muscle or at its endocardial surface. Ischemia and injection of
formaline produced local decrease or disappearance of electric
activity and local reversals of the direction of spread of activation
in limited portions of the papillary muscle or in the overlying wall
of the left ventricle.
Three types of aberrant spread
of activation in the papillary muscle during premature ventricular
contractions were described.
Publication:
1.
Spread of activation in the anterolateral papillary muscle of the left
ventricle of the dog under normal and pathologic conditions.
Burch GE, Wajszczuk WJ, Cronvich JA. Am
Heart J.
1970 Jun;79(6):769-88. |